
The endometrium is the lining of the uterus and plays a key role throughout the menstrual cycle. The thickness of the endometrium varies throughout the cycle based on factors such as hormones and often decides the chances of a successful pregnancy. Interpreting endometrial thickness may help understand the chances of conception.
Doctors often depend on monitoring of the endometrial thickness when helping patients with fertility problems. So, what exactly is endometrial thickness? What is its role in menstrual cycle and fertility and what are the parameters for normal endometrial thickness?
In This Article
- What is Endometrial Thickness?
- Significance of Normal Endometrial Thickness
- Factors Influencing Endometrial Thickness
- FAQ’s
What is Endometrial Thickness?
Endometrial thickness refers to the measurement of the lining of the uterus, known as the endometrium. This lining changes the menstrual cycle in response to hormonal fluctuations (1).
During The Menstrual Cycle
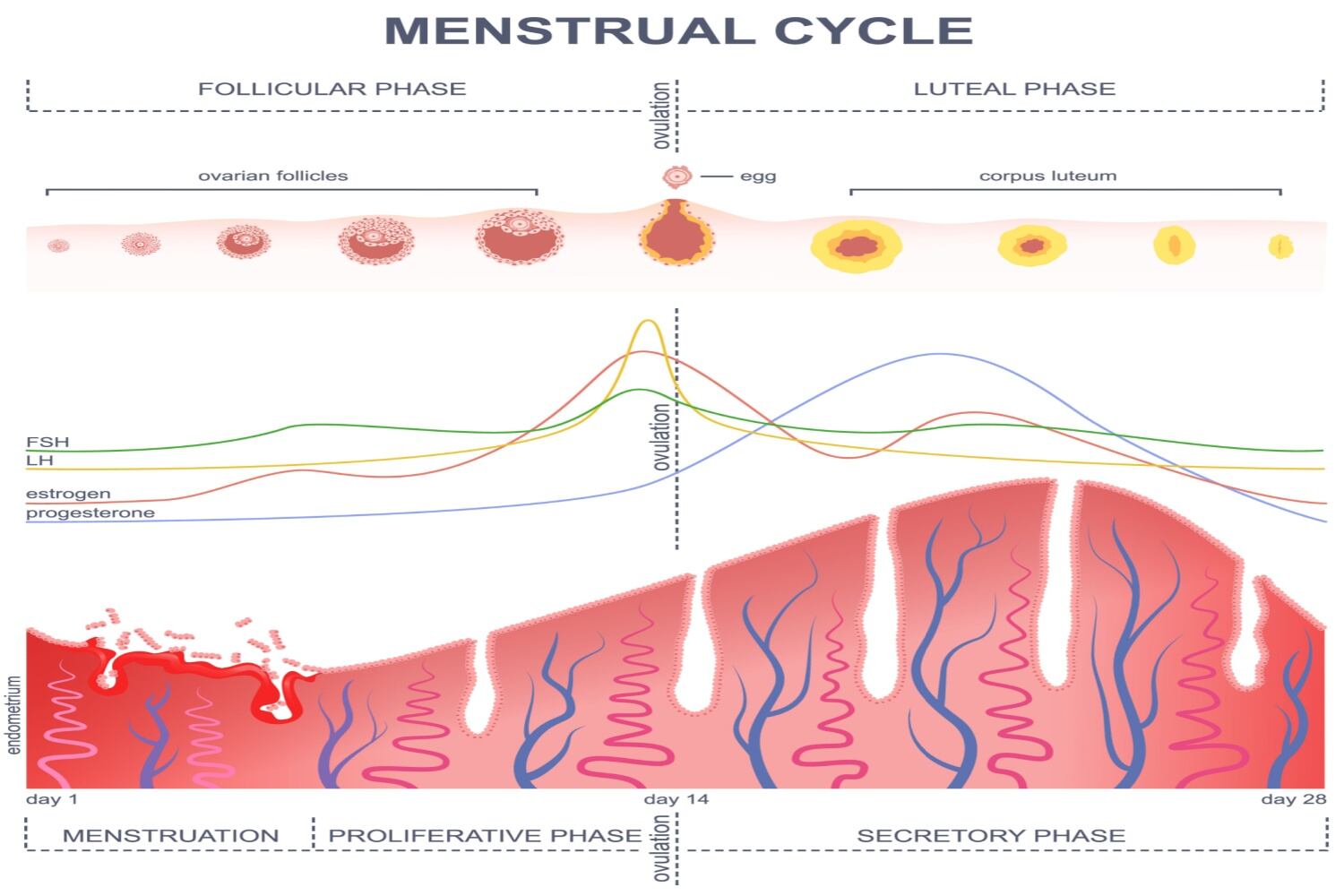
In the early part of the cycle (proliferative phase), the endometrium starts to thicken in response to estrogen.
Midway through the cycle, around ovulation, the endometrium continues to thicken under the influence of estrogen and progesterone.
In the latter part of the cycle (secretory phase), if pregnancy doesn’t occur, hormonal levels drop, leading to the shedding of the endometrial lining during menstruation (2).
Measuring endometrial thickness is often done through ultrasound imaging (3). It’s an essential part of evaluating reproductive health, especially in assessing fertility, investigating menstrual irregularities, and diagnosing certain gynecological conditions. If an ultrasound imaging does not help then a MRI is suggested.
After Menopause
In postmenopausal women, the endometrial lining typically becomes thinner due to the absence of menstrual cycles and hormonal changes. Abnormalities in endometrial thickness, whether excessively thin or thick, can sometimes indicate underlying medical conditions and may require further investigation by a healthcare professional (4).
[Read: Phases of Menstrual Cycle – A Comprehensive Guide]
Significance of Normal Endometrial Thickness

The significance of normal endometrial thickness lies in its role in reproductive health and overall wellness. Here are some key points
1. Fertility
- Crucial for Implantation: An optimal endometrial thickness is essential for successful embryo implantation during conception (5).
- Supports Pregnancy: A healthy endometrium provides an ideal environment for the fertilized egg to attach and grow.
2. Menstrual Health
- Regular Cycles: Normal endometrial thickness contributes to regular, healthy menstrual cycles.
- Balanced Hormones: It reflects a balance in hormone levels—estrogen and progesterone—necessary for endometrial growth and shedding during menstruation.
3. Postmenopausal Health
- Indicator of Changes: In postmenopausal women, a thin endometrium is expected and signifies the absence of menstrual cycles (6).
- Assessment for Health: It can be an indicator of overall postmenopausal health, as significant changes might warrant further investigation.
4. Reproductive Wellness
- Diagnostic Indicator: Abnormal endometrial thickness might be a clue for underlying conditions like polyps, fibroids, hormonal imbalances, or even endometrial cancer.
- Monitoring Tool: Regular assessment helps in tracking reproductive health and detecting potential issues early on.
5. Fertility Treatments
- Guide for Treatments: In assisted reproductive technologies (ART) like IVF, monitoring endometrial thickness is crucial to optimize the chances of successful implantation and pregnancy (7).
Understanding the importance of normal endometrial thickness is vital for assessing fertility, menstrual health, and overall reproductive wellness. Monitoring changes and seeking medical advice for any deviations from the norm ensures timely intervention and better management of potential reproductive health issues.
Factors Influencing Endometrial Thickness
Several factors influence endometrial thickness such as
1. Hormonal Fluctuations
Progesterone and estrogen are two hormones that are essential to the menstrual cycle. Estrogen stimulates endometrial growth, while progesterone helps maintain its thickness and prepares it for potential pregnancy.
Fluctuations in these hormones throughout the cycle influence endometrial thickness.
2. Menstrual Cycle Phases
Proliferative Phase: In the early part of the cycle, the endometrium starts thickening in response to rising estrogen levels (2A).
Secretory Phase: After ovulation, progesterone causes further thickening in preparation for a potential embryo implantation. If pregnancy doesn’t occur, the lining sheds during menstruation (2B).
3. Age
Endometrial thickness can vary with age. For example, in postmenopausal women, the endometrium typically becomes thinner due to decreased estrogen levels and the absence of menstrual cycles.
4. Medications And Hormone Therapies
Certain medications, including hormone replacement therapy and fertility treatments, can affect hormone levels and consequently impact endometrial thickness.
5. Medical Conditions
Polycystic Ovary Syndrome (PCOS): Hormonal imbalances in PCOS can lead to irregular thickening of the endometrium.
Endometrial Conditions: Conditions like endometrial hyperplasia, polyps, or fibroids can affect endometrial thickness.
6. Reproductive Health Intervention
In Vitro Fertilization (IVF) or Fertility Treatments: Monitoring endometrial thickness is crucial for optimizing the chances of successful embryo implantation.
The typical thickness of the endometrium changes throughout a person’s life, from childhood to puberty, through reproductive years, and after menopause.
[Read: Life With PCOD After Marriage – A Complete Guide]
The first half of the proliferative phase starts between days 5–14 of a person’s cycle, or the time between the end of one menstrual cycle, when bleeding stops, and before ovulation. The endometrium begins to thicken and may measure between 10–16 mm during this period. Hormones trigger the release of an egg in 14 days into a person’s cycle. The endometrial thickness is at its greatest at this time and can reach 18 mm.
Endometrial thickness is important in pregnancy. Healthcare professionals link the best chance of a full-term pregnancy when an endometrium is neither too thin nor too thick. This thickness allows the embryo to implant correctly and receive the nutrition it needs. The endometrium gets thicker as the pregnancy progresses.
Some reports state that 5% of people under 40 years old and 25% of people over 40 years old have thin endometrium.
Understanding these influences helps in interpreting changes in endometrial thickness and their implications for reproductive health. Consulting a healthcare provider can provide personalized insights and guidance regarding individual factors affecting endometrial health.
FAQ’s
1. What Can Cause Abnormal Endometrial Thickness?
Abnormal endometrial thickness may be due to many factors such as hormonal disturbances, polyps, and fibroids. In certain cases, abnormalities in the endometrium may also indicate cancer.
2. What Endometrial Thickness is Best For Conceiving?
Endometrial thickness of 10 mm and above is best for conceiving while a thickness of 7mm to 14 mm increases the chances of conception.
References
- The endometrium in assisted reproductive technology: How thin is thin? – PMC – [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4817285/]
- Physiology, Menstrual Cycle – StatPearls – NCBI Bookshelf – [https://www.ncbi.nlm.nih.gov/books/NBK500020/]
- The effect of endometrial thickness and pattern measured by ultrasonography on pregnancy outcomes during IVF-ET cycles – PMC- [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3551825/]
- How thick is too thick? When endometrial thickness should prompt biopsy in postmenopausal women without vaginal bleeding – PubMed – [https://pubmed.ncbi.nlm.nih.gov/15386607/]
- Ideal embryo transfer position and endometrial thickness in IVF embryo transfer treatment – PubMed – https://pubmed.ncbi.nlm.nih.gov/30238667/
- Understanding the Endometrium at Menopause: Magnetic Resonance Imaging: A Radiologist’s View – PMChttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC8409710/
- Should we continue to measure endometrial thickness in modern-day medicine? The effect on live birth rates and birth weight – ScienceDirecthttps://www.sciencedirect.com/science/article/abs/pii/S1472648317307113
