
As parents, we all want our children to lead happy, confident lives. However, when a child has frequent urination or an overactive bladder (OAB), it can pose a significant challenge for both them and the entire family. Frequent and sudden urges to urinate, often leading to accidents, can disrupt a child’s daily routine, causing stress and embarrassment. These moments not only impact their self-esteem but also affect their social interactions, making it harder for them to participate fully in school and play activities.
Dealing with frequent urination can feel overwhelming, but there are effective strategies to help manage the symptoms and improve the children’s quality of life. By understanding what OAB is and how to address it, we can support our children in gaining better bladder control and restoring their confidence. Together, we can navigate this journey and ensure our kids enjoy their childhood to the fullest.
What is an Overactive Bladder (OAB)?
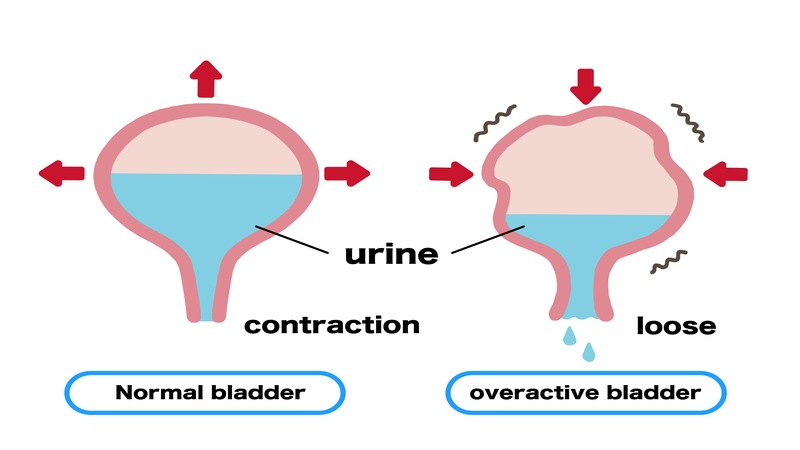
Overactive bladder (OAB) in children is a condition where there is a frequent and sudden urge to urinate that is challenging to control (1a). This urgency can lead to incontinence (unintentional loss of urine) which result in daytime wetting, bedwetting, or a combination of both, which can significantly impact a child’s daily activities, and quality of life. OAB mostly goes undiagnosed till the child turns 5-6 hears of age. As by the time a child turns 5, they are able to control their urine, especially during the day (2).
Signs of Overactive Bladder in Children

Overactive bladder in children is characterized by a combination of signs that disturb normal urinary function, including:
Urinary Frequency: The child needs to urinate more often than usual, typically more than eight times a day, disrupting daily activities.
Urgency: A sudden and strong need to urinate that can be difficult to control, often requiring the child to rush to the bathroom.
Urge Incontinence: Involuntary leakage of urine that occurs because the child cannot reach the bathroom in time after feeling a sudden urge to urinate.
[Read: Hematuria (Blood in Urine) in Children – Causes, Symptoms and Treatment]
What Causes Overactive Bladder in Children?

Overactive bladder in children can be caused by various factors that affect the normal function of the bladder and its control mechanisms. Some common causes include:
- The Neurogenic Theory: The brain sends fewer signals to stop the bladder from contracting and more signals telling it to contract, making the child feel the need to urinate more often (3).
- The Myogenic Theory: The bladder muscle becomes more sensitive and overactive, leading to more frequent, spontaneous contractions (4).
- The Autonomous Bladder Theory: The bladder becomes more active due to certain chemical signals, causing it to contract more frequently (5).
- The Afferent Signaling Theory: As the bladder fills, it contracts on its own, sending stronger signals to the brain about needing to urinate, making the child more aware of the bladder filling up (6).
When to See a Doctor?

You should see a doctor for overactive bladder in children if you notice any of the following:
- The child needs to pee very often
- There is a sudden, strong urge to pee that is hard to control
- The child has accidents and wets their clothes
- Bedwetting happens often
- The child feels pain when peeing
- There are big changes in how often or how much the child pees
- The child gets urinary tract infections (UTIs) often (7)
- The bladder problems make the child upset or embarrassed (1b)
How is Overactive Bladder Diagnosed in Children?

Overactive bladder in children can be diagnosed through a combination of medical history, physical examination, and possibly some tests. Here’s how it is typically diagnosed:
1. Medical History:
The doctor will ask detailed questions about the child’s symptoms, including frequency of urination, urgency (sudden need to urinate), and any incidents of urinary incontinence (accidental urination).
2. Physical Examination:
A physical examination may be performed to check for any signs of infection or abnormalities that could contribute to the symptoms.
3. Bladder Diary:
Keeping a bladder diary can provide valuable information (8). The child or caregiver records when and how much the child drinks, when they urinate, and any accidents that occur. This helps identify patterns and severity of symptoms.
4. Urinalysis:
A urine sample may be collected to check for signs of infection, blood, or other abnormalities in the urine.
5. Bladder Ultrasound:
In some cases, an ultrasound of the bladder may be performed to assess bladder capacity and to rule out any anatomical abnormalities.
6. Urodynamic Testing:
If necessary, urodynamic testing may be recommended. This involves various tests to evaluate how well the bladder and urethra store and release urine. These tests can help determine if the bladder muscle (detrusor) is overactive.
7. Other Tests:
Depending on the specific symptoms and suspected causes, additional tests such as blood tests or imaging studies may be ordered.
It’s important for the doctor to differentiate overactive bladder from other conditions that can cause similar symptoms, such as urinary tract infections, constipation, or anatomical abnormalities. Therefore, a thorough evaluation is crucial to make an accurate diagnosis and develop an appropriate treatment plan for the child.
[Read: Vaccination in Children With Immune Deficiency]
Overactive Bladder Treatment Options For Children
Using a combination of treatments that fit your child’s needs can really help improve symptoms and their quality of life when dealing with overactive bladder. It’s important for families to understand these options so they can set realistic goals for managing OAB effectively:
1. Behavioral and Lifestyle Changes:
- Bladder Training: Teaching the child to urinate at regular intervals to increase bladder capacity (9).
- Timed Voiding: Scheduling regular bathroom breaks to avoid urgency.
- Fluid Management: Encouraging regular fluid intake and reducing caffeine or sugary drinks that can irritate the bladder.
- Dietary Changes: Managing constipation with a high-fiber diet to reduce bladder pressure.
2. Medications:
- Antimuscarinic agents: Oxybutynin the only FDA-approved medication for children with OAB, which helps relax the bladder muscle (10).
- Other Medications: Sometimes, doctors might recommend other types of medications not specifically approved for children but can be effective under medical supervision.
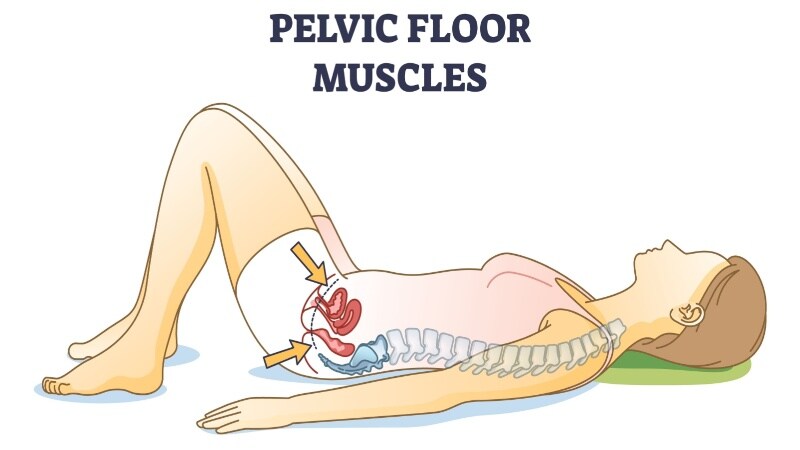
3. Pelvic Floor Exercises:
Exercises to strengthen the muscles that control urination, often guided by a healthcare professional (11).
4. Biofeedback:
A technique that helps children become aware of and control their bladder muscles through visual or auditory feedback (12).
5. Advanced Treatments (for severe cases):
- Injections: Injections into the bladder muscle can help reduce overactivity (1c).
- Electrical Stimulation: A procedure that uses electrical impulses to help regulate bladder function.
6. Education and Support:
- Providing information and support to the child and family to manage symptoms and set realistic expectations for treatment outcomes.
It’s important to consult a healthcare professional to determine the most appropriate medication and dosage for a child’s specific needs. The choice of medication may depend on the child’s symptoms, medical history, and response to treatment.
Home Remedy For Frequent Urination in Children

Changes in your child’s routines can help improve bedwetting. Encourage your child to:
- Drink most liquids in the morning and early afternoon
- Go to the bathroom regularly during the day—every 2 to 3 hours—and just before bed
- Go to the bathroom twice before bedtime (about 30 minutes apart) to fully empty the bladder
- Avoid drinks with caffeine, bubbles, citrus juices, and sports drinks, as they can irritate the bladder and produce more urine
Dealing with an overactive bladder in children can be challenging, but taking a comprehensive approach can make a big difference. By using behavioral strategies, considering medications when necessary, and offering ongoing support, we can help our children manage their symptoms more effectively. It’s important to work closely with healthcare providers to get the right tools and knowledge, which can greatly improve our children’s quality of life and bladder health. Ongoing research and advancements give us hope for even better treatments in the future, making life easier for our kids and us.
FAQ’s
1. Are Overactive Bladder And Urinary Incontinence Same?
Overactive bladder and urinary incontinence are related but NOT identical. OAB involves sudden, uncontrollable urges to urinate, often leading to urinary incontinence (leakage). However, urinary incontinence can occur due to various reasons beyond OAB, such as stress incontinence (leakage during physical exertion) or overflow incontinence (incomplete bladder emptying).
2. Is Bedwetting Related to Overactive Bladder in Children?
Bedwetting (nocturnal enuresis) can be related to overactive bladder in children, but it’s not always the case. Overactive bladder can contribute to nocturnal enuresis by increasing bladder activity and urgency during sleep. However, bedwetting can also be caused by other factors such as delayed bladder maturation, genetic predisposition, or emotional stress.
3. Can a Child Have Frequent Urination But no UTI?
Yes, a child can experience frequent urination without having a urinary tract infection (UTI). Overactive bladder, excessive fluid intake, anxiety, or certain medications can cause frequent urination. It’s important to differentiate between these causes through a medical evaluation to determine appropriate management.
4. What Foods Stop Urination?
To help reduce frequent urination in children, focus on giving them low-acid fruits like bananas and blueberries, lean proteins like chicken, and whole grains like brown rice. Avoid giving them caffeinated drinks, spicy foods, and citrus fruits, which can irritate the bladder.
5. Can Anxiety Cause Excessive Urination in Kids?
Yes, anxiety can cause excessive urination in kids. Emotional stress and anxiety can lead to heightened nervous system activity, affecting bladder function and increasing urinary frequency. Addressing anxiety through counseling, relaxation techniques, or other interventions may help alleviate associated urinary symptoms.
Read Also: Heart Murmur in Kids – Everything You Need to Know
References
- Ramsay S, Bolduc S. Overactive bladder in children. Can Urol Assoc J. 2017 Jan-Feb;11(1-2Suppl1):S74-S79. doi: 10.5489/cuaj.4337. PMID: 28265325; PMCID: PMC5332242. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5332242/
- National Institute of Diabetes and Digestive and Kidney Diseases – https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-bedwetting-children/definition-facts
- de Groat WC. A neurologic basis for the overactive bladder. Urology. 1997 Dec;50(6A Suppl):36-52; discussion 53-6. doi: 10.1016/s0090-4295(97)00587-6. PMID: 9426749. – https://pubmed.ncbi.nlm.nih.gov/9426749/
- Brading AF. Spontaneous activity of lower urinary tract smooth muscles: correlation between ion channels and tissue function. J Physiol. 2006 Jan 1;570(Pt 1):13-22. doi: 10.1113/jphysiol.2005.097311. Epub 2005 Oct 6. PMID: 16210349; PMCID: PMC1464291. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1464291/
- Drake MJ, Mills IW, Gillespie JI. Model of peripheral autonomous modules and a myovesical plexus in normal and overactive bladder function. Lancet. 2001 Aug 4;358(9279):401-3. doi: 10.1016/s0140-6736(01)05549-0. PMID: 11502339. – https://pubmed.ncbi.nlm.nih.gov/11502339/
- Andersson KE. Detrusor myocyte activity and afferent signaling. Neurourol Urodyn. 2010;29(1):97-106. doi: 10.1002/nau.20784. PMID: 20025035. – https://pubmed.ncbi.nlm.nih.gov/20025035/
- Shim J, Oh MM. Updates of Overactive Bladder in Pediatrics. Int Neurourol J. 2023 Mar;27(1):3-14. doi: 10.5213/inj.2244228.114. Epub 2023 Mar 31. PMID: 37015720; PMCID: PMC10073000. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10073000/
- Locher JL, Goode PS, Roth DL, Worrell RL, Burgio KL. Reliability assessment of the bladder diary for urinary incontinence in older women. J Gerontol A Biol Sci Med Sci. 2001 Jan;56(1):M32-5. doi: 10.1093/gerona/56.1.m32. PMID: 11193230. – https://pubmed.ncbi.nlm.nih.gov/11193230/
- National Institute of Diabetes and Digestive and Kidney Diseases – https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-bedwetting-children/treatment
- The National Health Service – https://www.nhs.uk/medicines/oxybutynin/
- Leron E, Weintraub AY, Mastrolia SA, Schwarzman P. Overactive Bladder Syndrome: Evaluation and Management. Curr Urol. 2018 Mar;11(3):117-125. doi: 10.1159/000447205. Epub 2018 Feb 20. PMID: 29692690; PMCID: PMC5903463. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5903463/
- Krzemińska K, Maternik M, Drożyńska-Duklas M, Szcześniak P, Czarniak P, Gołębiewski A, Zurowska A. High efficacy of biofeedback therapy for treatment of dysfunctional voiding in children. Cent European J Urol. 2012;65(4):212-5. doi: 10.5173/ceju.2012.04.art6. Epub 2012 Dec 11. PMID: 24578964; PMCID: PMC3921803. – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3921803/

