 The human body is prone to get infected by bacteria and bugs around us. A good diet and proper hygiene practices help to allay such infections. These bacteria can easily affect the female reproductive organs. One such condition causing infection of the female genital tract is Pelvic Inflammatory Disease. Taking good care of intimate areas along with healthy sexual practices keeps such infections away.
The human body is prone to get infected by bacteria and bugs around us. A good diet and proper hygiene practices help to allay such infections. These bacteria can easily affect the female reproductive organs. One such condition causing infection of the female genital tract is Pelvic Inflammatory Disease. Taking good care of intimate areas along with healthy sexual practices keeps such infections away.
The clinical presentation of PID differs from woman to woman. Some remain asymptomatic, while a few suffer from severe symptoms. If left untreated, it can lead to certain complications, including infertility. Infertility due to PID can be a very challenging issue, and one needs to address it as early as possible.
In This Article
- What is Pelvic Inflammatory Disease?
- How Does Pelvic Inflammatory Disease Affect Fertility?
- Top 5 Causes of Pelvic Inflammatory Disease
- Signs And Symptoms of Pelvic Inflammatory Disease
- How is PID Diagnosed?
- PID Treatment For Women
- How Can PID Be Prevented?
- Possible Complications That May Occur in PID
- When Should You Consult a Doctor?
- FAQ’s
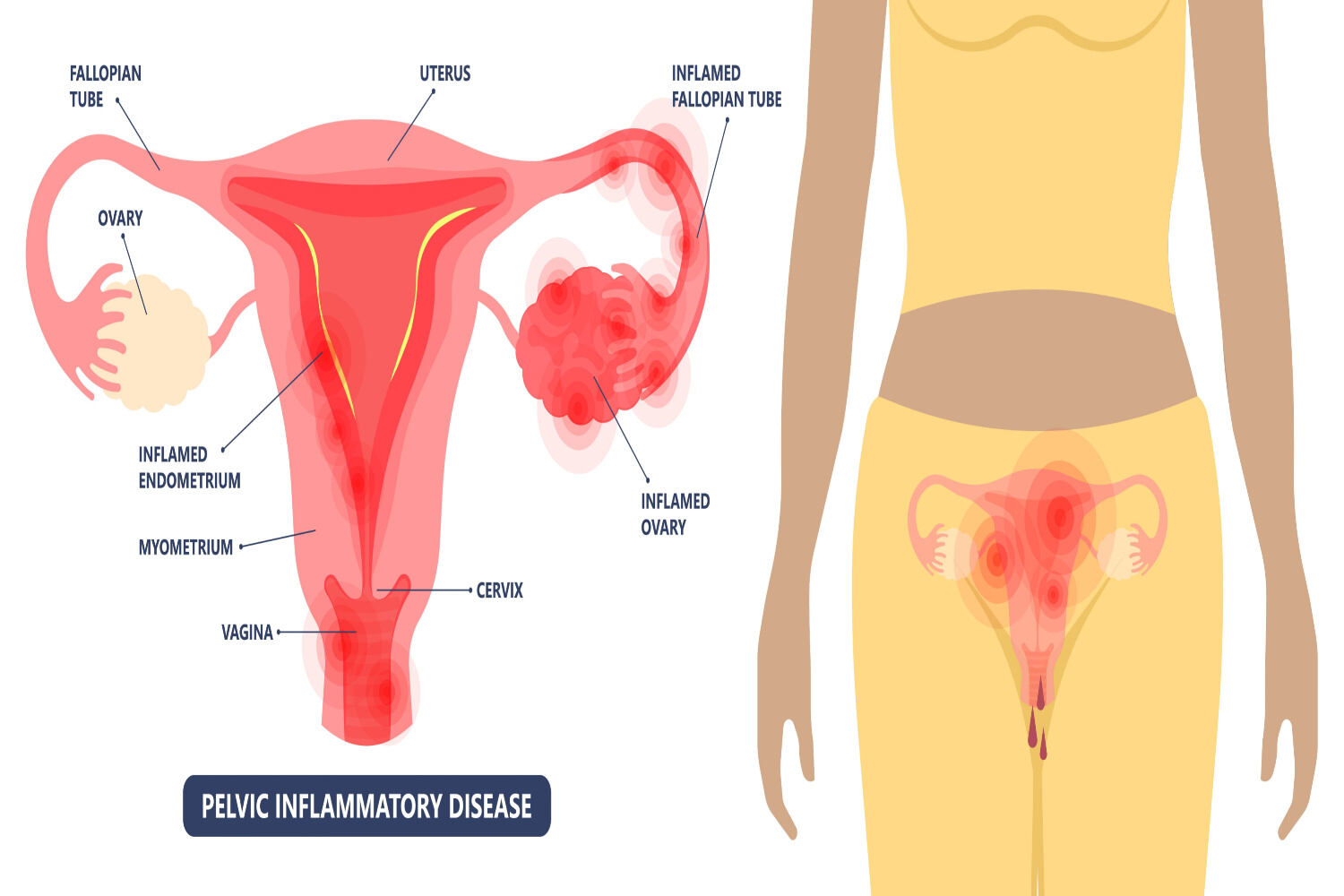
What is Pelvic Inflammatory Disease?
Pelvic Inflammatory disease is an infection of the upper female genital tract involving the uterus, fallopian tubes, or ovaries. It mostly affects young women in the reproductive age group. Sexually transmitted infections(STIs) like chlamydia, and and gonorrhea are the most common cause of PID. In 2019, 1.05 million reproductive-aged women had active PID globally [1].
How Does Pelvic Inflammatory Disease Affect Fertility?

Pelvic inflammatory disease or PID is one of the major causes of infertility with 1 in 8 women experiencing difficulty conceiving due to PID-related factors and complications [2]. PID is most commonly seen in girls and women between 15 to 25 years of age.
The most common manifestation of PID is an infection in the upper genital tract that can cause infection, inflammation,, and scarring. The epithelial cells lining the fallopian tube can get blocked which can result in impaired movement of the ovum during the process of fertilization. This can result in total infertility or ectopic pregnancy [3].
Tubal factor infertility and ectopic pregnancy are the most common consequences of PID [4] and can cause infertility and difficulty conceiving in the long run. While tubal factors account for around 25%-35% of cases of infertility, PID is responsible for more than half of these cases [5].
It is also important to remember that recurrent PID infections can result in more severe tubal dysfunctions [5A] which may even lead to permanent infertility.
Top 5 Causes of Pelvic Inflammatory Disease
 Bacterial infection is the most common culprit for Pelvic Inflammatory Disease. These organisms often ascend up to the upper genital tract. The most common causes of PID are bacteria like Chlamydia trachomatis, Neisseria gonorrhea, and Mycoplasma genitalium [3A]. Mostly, gonorrheal PID is more severe than PID due to chlamydia or other causes. Less severe cases lead to fewer symptoms resulting in subclinical PID. Other known causes are:
Bacterial infection is the most common culprit for Pelvic Inflammatory Disease. These organisms often ascend up to the upper genital tract. The most common causes of PID are bacteria like Chlamydia trachomatis, Neisseria gonorrhea, and Mycoplasma genitalium [3A]. Mostly, gonorrheal PID is more severe than PID due to chlamydia or other causes. Less severe cases lead to fewer symptoms resulting in subclinical PID. Other known causes are:
1. Unprotected Sexual Intercourse With Multiple Sexual partners
Bacteria easily transmit while one has intercourse without the use of condoms. Inconsistent condom use was significantly associated with a 2-3 times elevated risk for upper genital tract infection [3B]. There is always a risk of passing on infection in case of multiple partners.
2. History of Abortions
Medical abortion or surgical abortion can result in infection as the cervix opens up during an abortion, which allows bacteria to ascend.
3. Poor Menstrual Hygiene
Maintaining improper hygiene during periods can be a cause. The use of tampons for a long time contributes more to the infection.
4. Vaginal Douching
Frequent use of soap around the intimate area leads to an imbalance in the normal vaginal flora. A literature review suggests that vaginal douching is a risk factor for PID [6].
5. Intrauterine Device
The first few weeks following Intrauterine device (IUD) insertion can be a cause of infection. The WHO Medical eligibility criteria for contraceptive use state that IUD insertion increases the risk of PID among women at increased risk of sexually transmitted infections.
Signs and Symptoms of Pelvic Inflammatory Disease
Some women show only a few symptoms or remain asymptomatic for a long time. Some experience severe symptoms in a short duration of time. The usual signs and symptoms [3C] are:
- Lower abdominal pain and discomfort. It could be unilateral or bilateral, depending on whether one or both sides of the tubes and ovaries are involved.
- Heavy, abnormal vaginal discharge with an unpleasant odor.
- Irregular menstrual cycles with or without dysmenorrhea.
- Painful intercourse, also known as dyspareunia. In a few cases, there might be bleeding following sex.
- Fever along with chills in a few severe cases.
How is PID Diagnosed?
 A thorough personal, menstrual, and sexual history is very important in reaching the diagnosis. Physical examination to look for any abdominal tenderness or pelvic mass can help in early detection. Additional tests include-
A thorough personal, menstrual, and sexual history is very important in reaching the diagnosis. Physical examination to look for any abdominal tenderness or pelvic mass can help in early detection. Additional tests include-
- Vaginal swabs to test for gonorrhea and Chlamydia. Nucleic acid amplification tests (NAAT) for N.gonorrhoeae and C.trachomatis must be done for all patients.
- Blood tests to look for white blood cell count as it rises in infections. ESR and CRP can be done to rule out inflammation.
- Urine pregnancy test to rule out any ectopic pregnancy.
- Test to rule out HIV and other STIs.
- Digital examination, including abdominal or transvaginal ultrasound to view the health of the pelvis. An ultrasound can help to visualize the tubo-ovarian mass.
- Laparoscopic examination might be needed in a few cases for better visualization of the internal organs. For tissue culture and histology, an endometrial biopsy can also help.
PID Treatment For Women
Any of the above symptoms require quick medical action to lessen the complications. Until the infection is gone it is best to maintain sexual abstinence. With the use of broad-spectrum antibiotics doctors mostly treat PID. Few patients don’t respond well to oral antibiotics. IV antibiotics are often a better option for those [3D]. Sexual partners must also be assessed for infection and treated accordingly. In complicated cases, one may require surgery.
How Can PID Be Prevented?
 Prevention aims at reducing the risk factors. There must be more awareness at a primary level by creating awareness in the general population. Some of the preventive measures are as follows
Prevention aims at reducing the risk factors. There must be more awareness at a primary level by creating awareness in the general population. Some of the preventive measures are as follows
- Blood Tests and regular screening for STIs.
- Use of a barrier method of contraception. Condom use prevents contracting STDs [7].
- Limiting the number of sexual partners.
- Limiting the use of soap to wash the external genitalia as douching leads to an imbalance in the good and bad bacteria in the vagina.
- Encouraging sexual partners for frequent testing for STIs.
Possible Complications That May Occur in PID
Timely intervention can be helpful to limit the damage. Usually, it is treated well with antibiotics. Few women develop a certain complications if left untreated.
1. Ectopic Pregnancy
It is when the implantation of the fertilized egg occurs at sites other than the uterus. Fallopian tubes are the most common site. If infection leads to scarring of the lining of tubes, then it increases the chances of an ectopic. This can be life-threatening and requires quick medical intervention.
2. Infertility
Difficulties in conceiving might arise, as there could be permanent damage or scarring to some of the vital organs. A scarred endometrial lining or a blocked fallopian tube will hamper the chances of getting pregnant. Infertility related to PID is more likely to occur if chlamydia is the cause.
3. Premature Birth
If the woman conceives despite the infection, the chances of a premature delivery are quite high owing to the inflammation and scarring.
4. Recurrence of Infection
Recurrent Pelvic Inflammatory Disease can happen if one does not complete the course of antibiotics. Also in cases where the partner remained untreated.
5. Tubo-Ovarian Abscess
Sometimes in severe infection, pus collects over time. This mostly happens around the fallopian tubes and the ovaries, which require drainage.
When Should You Consult a Doctor?

If you have had a history of PID and are planning to conceive or having difficulty conceiving, you may need to consult a doctor or a fertility specialist. PID can cause ectopic pregnancy. Since tubal scarring and blocked fallopian tubes are common with PID, conception may get difficult.
Treating any underlying infections and checking for damage to the reproductive system is vital to being able to get pregnant. Fertility specialists may resort to ARTs such as IVF to help achieve pregnancy.
Conception with PID may be difficult but not impossible. Pelvic Inflammatory Disease is treatable if diagnosed at an early stage. Regular screening and testing for STIs greatly helps in avoiding their spread to others. Encouraging partners to have regular assessments to have a healthy sexual relationship. A timely diagnosis and treatment helps to avoid the dreaded complications of ectopic pregnancy and infertility.
FAQ’s
1. How Long Does PID Last?
The infection usually clears up in a few days after the completion of an antibiotic course of 14 days. In case of surgical procedure then it will take almost 4-6 weeks for complete healing.
2. What Color is PID Discharge ?
It could be yellow, greenish or white with an unpleasant or a fishy odour. The vaginal discharge is quite thick in cases of PID.
References-
- Global burden of pelvic inflammatory disease and ectopic pregnancy from 1990 to 2019
[https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-16663-y] - STD Facts – Pelvic Inflammatory Disease [https://www.cdc.gov/pid/about/index.html]
- Pelvic Inflammatory Disease
[https://www.ncbi.nlm.nih.gov/books/NBK499959/] - Pelvic Inflammatory Disease and Infertility in Women – ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0891552020301033]
- RACGP – Pelvic inflammatory disease and infertility [https://www1.racgp.org.au/ajgp/2023/april/pelvic-inflammatory-disease-and-infertility]
- Vaginal douching as a possible risk factor for pelvic inflammatory disease.
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2625960/] - Emergency contraception
[https://www.who.int/news-room/fact-sheets/detail/emergency-contraception]

