Umbilical cord prolapse is a rare yet significant twist in the birthing journey, where the baby’s lifeline, the umbilical cord, takes an early plunge into the birth canal. Sounds a bit tricky, right? Well, it’s not super common, but it’s good to know about it.
Understanding what it is, its causes, and gaining insights into it is not just informative but empowering for expectant mothers. So, we’ll talk about what causes it and some smart ways to handle it, all in a simple and easy way. Because understanding this adds an extra layer of confidence to your pregnancy journey!
In This Article
- What Is an Umbilical Cord Prolapse?
- Types Of Umbilical Cord Prolapse
- Signs And Symptoms Of An Umbilical Cord Prolapse
- Causes Of An Umbilical Cord Prolapse
- Complications Of An Umbilical Cord Prolapse
- How Is Umbilical Cord Prolapse Diagnosed?
- Tips To Help You Manage Cord Prolapse
- Treatment Options For Cord Prolapse
- Can Cord Prolapse Be Prevented?
- FAQ’s
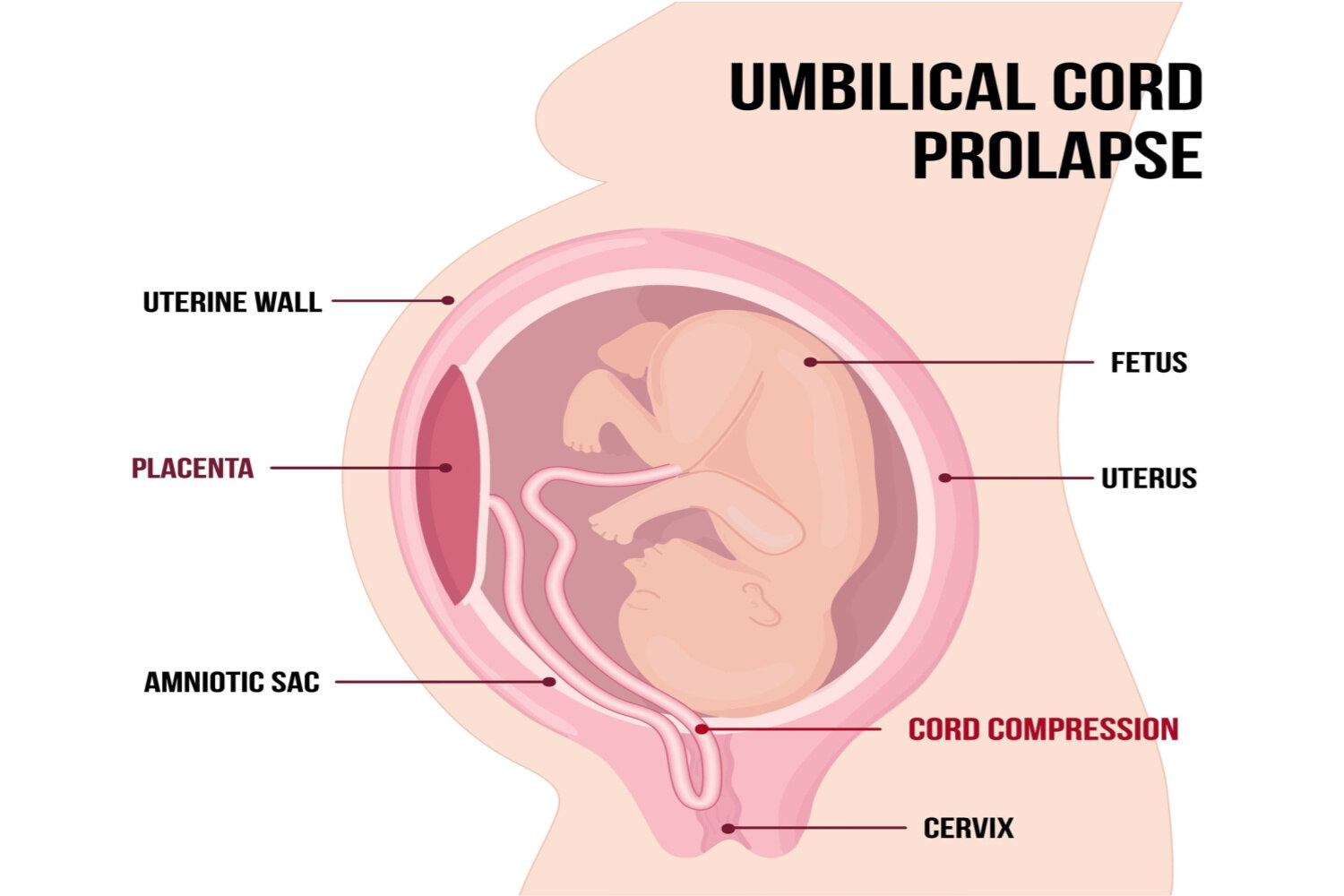
What Is an Umbilical Cord Prolapse?
The umbilical cord serves as a vital connection, acting as a lifeline between your unborn baby and the placenta. Its role involves transporting oxygen-rich blood and essential nutrients to the baby while efficiently removing waste. However, umbilical cord prolapse occurs when the cord slips into the vagina prematurely, before the baby is ready for birth.
This situation poses the risk of compression between the baby and pelvic bones, potentially reducing blood supply and oxygen levels. To mitigate these risks, swift delivery becomes imperative, aiming to prevent complications associated with decreased oxygen levels. Recognizing and addressing this issue promptly is crucial for ensuring the well-being of both the mother and the unborn child.
Types Of Umbilical Cord Prolapse
Childbirth envisioned as a journey, occasionally throws in surprises, and one such unexpected turn is cord prolapse, akin to the baby’s lifeline, the umbilical cord, getting a bit tangled in the journey’s twists. Understanding these twists is paramount for a safe and smooth delivery.[ 1 ]
Here are the twists in the journey, and the types of umbilical cord prolapse :
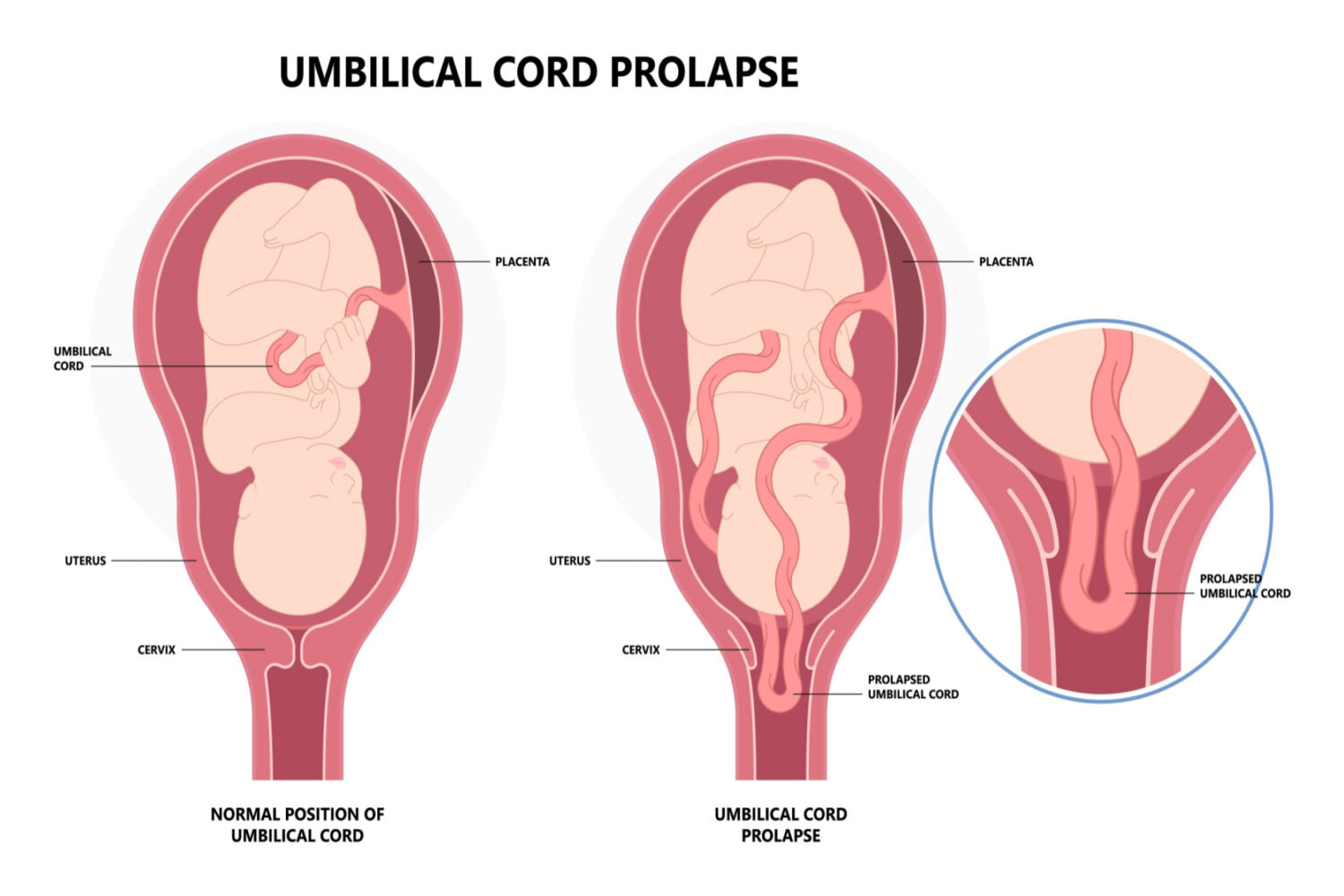
Overt Prolapse
In this type of prolapse, the cord slips out before the baby’s grand entrance. You might feel a pulsing sensation in the vaginal area. Diagnosis involves checking for this pulsing, often associated with potential issues in the baby’s heart rate.
Occult Prolapse
In this type, the cord slips out with the baby’s arrival. However, it can’t be seen or felt during routine checks. Diagnosis focuses on abnormal changes in the baby’s heart rate, especially when there’s no visible or felt cord. This assessment becomes critical after membrane rupture or other intricate procedures.
Like any journey, being aware of these twists ensures a more informed and prepared approach, contributing to a safer delivery experience for both the mother and the baby.
Signs And Symptoms Of An Umbilical Cord Prolapse
During childbirth, there’s a chance that the umbilical cord can misbehave, causing potential issues. Recognizing the signs and symptoms is crucial to prompt intervention by healthcare professionals, ensuring the safety of both the mother and the baby.
Watch out for these signs and symptoms [ 2 ] of cord prolapse:
- Feeling something down there: If you feel something in your vagina, it might be the cord.
- Seeing the cord: Sometimes, you might see the cord coming out.
- Doctor or midwife checks: Your healthcare provider could see or feel the cord during a check.
- Baby’s heart rate slows down: If the baby’s heart rate slows soon after your water breaks, it could mean the cord is squeezed, and the baby needs attention.
- No obvious signs: In some cases, there might not be any clear signs, so it’s essential to stay aware during check-ups and labor.
By recognizing and promptly addressing these signs, healthcare teams can implement appropriate measures, contributing to a safer and more controlled childbirth experience.
Causes Of An Umbilical Cord Prolapse
 Recognizing that umbilical cord prolapse has multiple causes, rather than just one, is essential to understanding it. While it frequently occurs after the water breaks, several critical contributors play a role in this complication during pregnancy. [ 1 ] [ 2 ] [ 3 ]
Recognizing that umbilical cord prolapse has multiple causes, rather than just one, is essential to understanding it. While it frequently occurs after the water breaks, several critical contributors play a role in this complication during pregnancy. [ 1 ] [ 2 ] [ 3 ]
- Breech presentation: Baby arriving feet-first.
- Polyhydramnios: Too much fluid around the baby.
- Premature rupture: Waters breaking early.
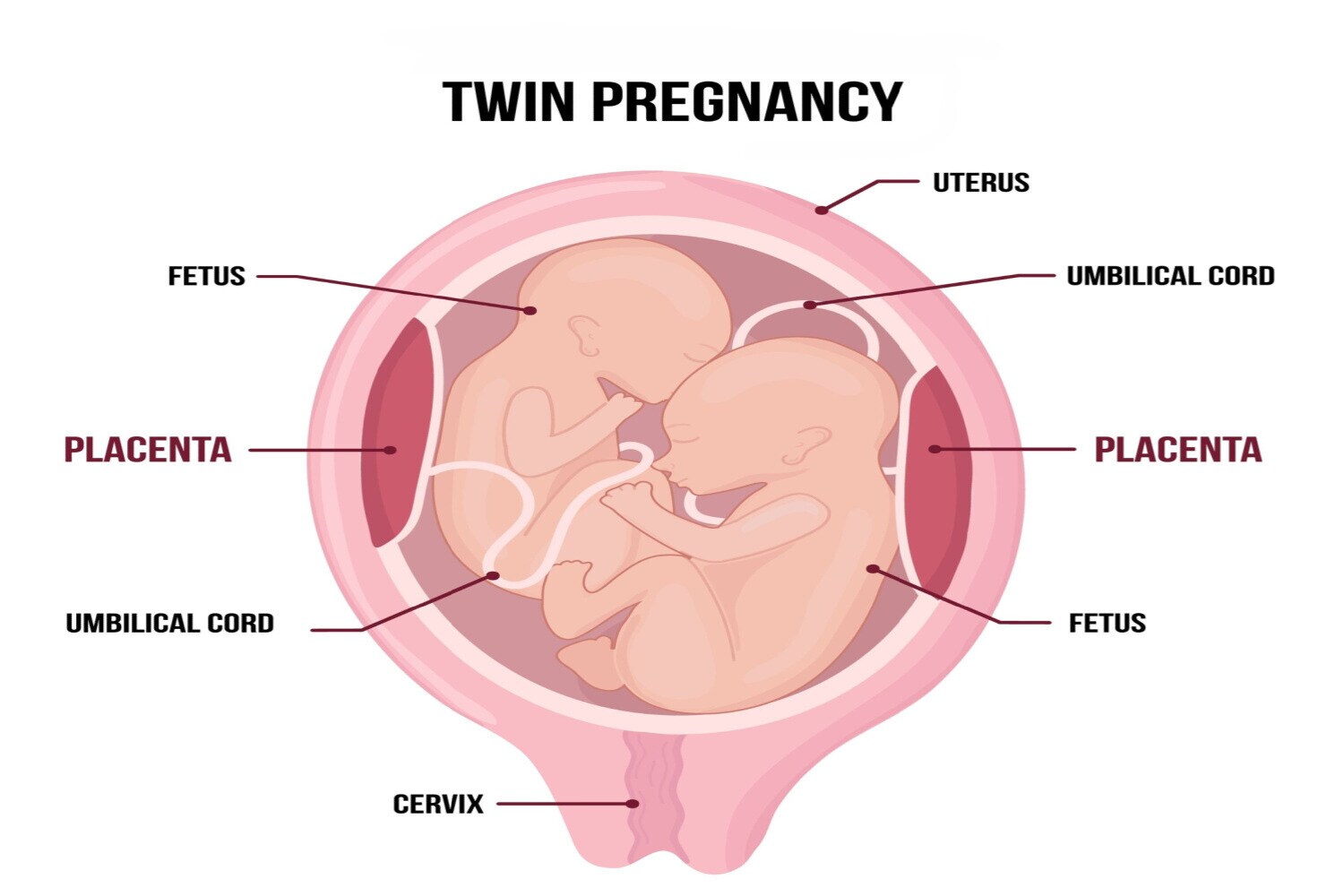
- Multiple pregnancies: More than one baby on the scene.
- Engagement and prolapse: The chance of cord prolapse decreases when the baby is comfortably settled in the pelvis. However, if the baby hasn’t moved into position, there’s room for the cord to slip and become problematic. Hence, ensuring the baby is snug equals a safer delivery.
In this narrative, each element adds suspense, requiring healthcare providers and parents to navigate with caution, anticipation, and meticulous care to ensure a safe and successful childbirth.
Complications Of An Umbilical Cord Prolapse
When the baby’s umbilical cord faces challenges during birth, it can lead to various issues. Let’s break it down [ 1 ]:
- Breathing trouble for the baby [Fetal Hypoxia]: Compression of the umbilical cord can lead to reduced oxygen supply to the fetus.
- Signs of baby distress [Fetal Distress]: Prolonged compression may result in fetal distress, reflected in abnormal heart rate patterns.
- Worst-case scenario [Fetal Mortality]: In severe cases, prolonged or untreated cord prolapse can lead to fetal death.
- Breathing problems for surviving babies [Neonatal Asphyxia]: Surviving infants may experience oxygen deprivation during delivery, leading to asphyxia.
- Possible brain issues [Neonatal Encephalopathy]: Lack of oxygen can cause brain injury, potentially resulting in neonatal encephalopathy.
- Cerebral palsy: Severe cases of asphyxia may contribute to the development of cerebral palsy in the infant.
- Emergency interventions: Complications may necessitate emergency interventions, including prompt delivery or cesarean section.
It’s important to note that complications vary in severity, and timely medical attention significantly influences outcomes.
How Is Umbilical Cord Prolapse Diagnosed?

Umbilical cord prolapse is akin to a mystery that doctors unravel using their detective skills, piecing together clues through a combination of observation, touch, and listening to the baby’s heartbeat.[ 4 ]
Here’s how the Diagnosis of Umbilical Cord Prolapse (UCP) unfolds:
- Overt UCP: Clear-cut scenario, seen or felt during a vaginal exam.
- Occult UCP: Trickier, with abnormal fetal heart rate patterns often being the first sign.
Diagnosis relies on clinical assessment, with no radiographic or laboratory confirmation. Diagnosis acts as the guiding compass through uncertainty, unveiling hidden chapters of the pregnancy journey and allowing for timely interventions that safeguard the precious moments of new beginnings.
Tips To Help You Manage Cord Prolapse
Dealing with prolapsed umbilical cord requires a strategic and prompt response to ensure the well-being of both the mother and the baby. Here are practical tips for managing cord prolapse: [ 1 ][ 4 ]
Quick Tips for Managing Cord Prolapse
- Call for Help: Notify your healthcare team immediately if you suspect cord prolapse. Cord prolapse is an emergency; seek immediate medical attention.
- Change Positions: Get on hands and knees or use a knee-chest position to relieve pressure.
- Stay Calm, Breathe Deeply: Keep calm and focus on slow, deep breaths to manage stress.
- Avoid Pushing: Refrain from pushing during contractions to prevent further cord compression.
- IV Fluids: Your healthcare provider may administer fluids to address any blood pressure drop.
- Continuous Monitoring: Keep a close eye on the baby’s heart rate for signs of distress.
- Prepare for Cesarean Section: Be ready for a cesarean section if recommended by your healthcare team.
Remember, follow the specific guidance of your healthcare professionals for your situation. Quick and coordinated actions are crucial in managing cord prolapse.
Treatment Options For Cord Prolapse

When confronted with visible umbilical cord situations during childbirth, the importance of swift and precise actions cannot be overstated. This critical scenario demands immediate attention to safeguard both the baby and the mother. [ 1 ]
- Delivery priority: Swift cesarean section is the go-to for cord prolapse, Rarely, quick vaginal delivery may be an option.
- Manual relief techniques: The doctor may insert their hand or fingers into the vagina to gently lift the baby part, compressing the cord.
- Bladder filling: Doctors may fill the bladder with a saline solution to mitigate cord pressure.
The chosen method depends on gestational age or maternal preference, with dilation, evacuation, or labor induction as options.
Can Cord Prolapse Be Prevented?
No magic wand for preventing this issue. But if you’re at a higher risk because your baby is doing somersaults or playing hide-and-seek with their position, the doctor might suggest being admitted to the hospital at week 37. It’s like a precautionary measure. [ 5 ] [ 6]
A prolapsed umbilical cord presents a unique challenge in childbirth, but informed choices and timely actions can greatly influence the course of childbirth. Recognizing risk factors, such as fetal positioning, and being proactive in seeking medical advice during pregnancy contribute to a safer delivery. While it’s essential to acknowledge that absolute prevention may not be possible, the emphasis on education, regular check-ups, and immediate response to potential complications can significantly enhance the chances of a positive outcome for both the baby and the mother. In navigating the complexities of childbirth, a collaborative approach between healthcare providers and expectant parents remains paramount.
FAQ’s
1. Is Cord Prolapse an Emergency?
Yes, cord prolapse is considered a medical emergency. Prompt intervention is crucial to prevent complications such as fetal distress, oxygen deprivation, or stillbirth.
2. Is Umbilical Cord Prolapse Common?
No, umbilical cord prolapse is not common. It is considered a rare but serious complication during pregnancy that demands immediate medical attention.
3. What are the Indications of Cord Prolapse?
The indications of cord prolapse include a sudden reduction in the baby’s heart rate, and the presence of a visible or palpable cord in the birth canal. Immediate medical attention is essential in addressing this situation promptly.
4. Which Position Is Best For Cord Prolapse?
It’s “Lefty Limbo” time! Just cozy up on your left side, let your head take the lead, and pop a pillow under your left hip or, play the “Knee-Chest Knight”. Because in childbirth, even your positions get a big cheer!
References
- Umbilical Cord Prolapse
[https://www.ncbi.nlm.nih.gov/books/NBK542241/] - Umbilical cord prolapse in late pregnancy
[https://www.rcog.org.uk/for-the-public/browse-our-patient-information/umbilical-cord-prolapse-in-late-pregnancy/] - Umbilical Cord Prolapse
[https://my.clevelandclinic.org/health/diseases/12345-umbilical-cord-prolapse#symptoms-and-causes] - Optimal management of umbilical cord prolapse
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6109652/] - Umbilical cord prolapse in late pregnancy
[https://www.rcog.org.uk/for-the-public/browse-our-patient-information/umbilical-cord-prolapse-in-late-pregnancy/] - Prevention of umbilical cord prolapse in high-risk patients
[https://www.ajog.org/article/S0002-9378(22)00547-6/fulltext]

